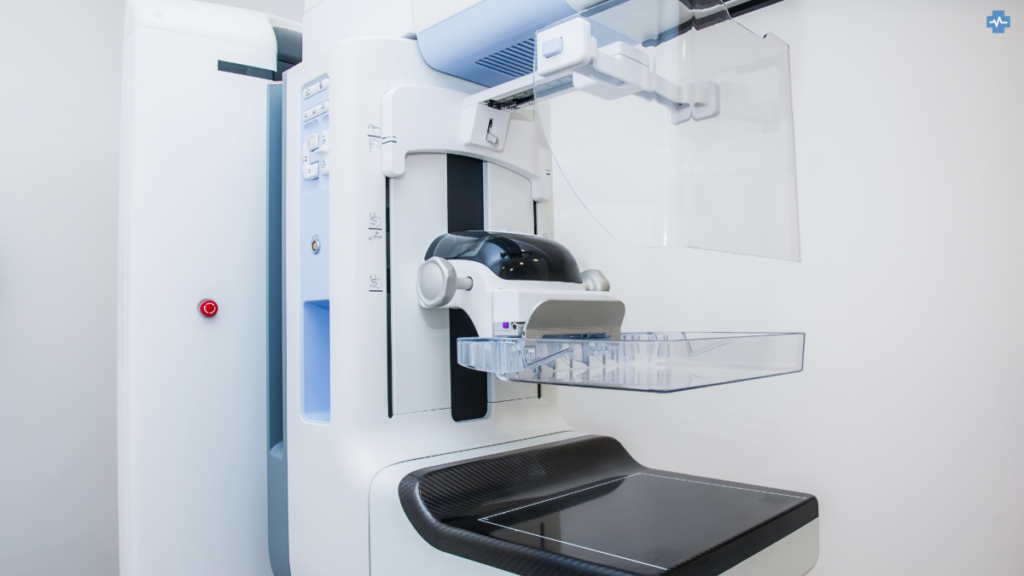
Digital Breast Tomosynthesis (DBT), commonly known as 3D mammography, represents a major leap forward in breast cancer diagnostics. Similar to how MRI is used in various areas such as brain imaging, cardiology, and musculoskeletal scans, DBT offers enhanced accuracy by providing high-resolution, multi-angle views of breast tissue. While traditional 2D mammograms capture only a single, flat image, DBT takes multiple X-ray images from different angles and reconstructs them into thin, detailed slices that offer a much clearer, three-dimensional view of the breast tissue.
How Does DBT Work?
Digital Breast Tomosynthesis (DBT) utilises low-dose X-rays to capture multiple images of the breast from different angles. These images are then reconstructed into thin, 1 mm slices, offering a detailed, layered view of the breast tissue. By allowing radiologists to examine breast tissue slice by slice, DBT significantly reduces the issue of tissue overlap, a common challenge in traditional 2D mammography. In standard 2D images, overlapping tissues can either hide small tumours or mimic abnormalities, leading to either missed cancers or false positives that result in unnecessary stress and further tests. DBT overcomes this by providing radiologists with clearer, more detailed images that improve diagnostic accuracy.
The ability to view the breast tissue in slices also benefits women with dense breast tissue, where traditional mammograms are often less effective. Dense tissue can obscure cancerous lesions on 2D mammograms, making it harder to detect abnormalities. In contrast, DBT’s detailed, layer-by-layer approach improves the visualisation of both small tumours and subtle abnormalities that might otherwise go unnoticed. Studies have shown that this technology increases the detection rate of breast cancer, particularly in women with dense breasts, and reduces the number of false positives, improving overall screening outcomes and reducing the need for unnecessary biopsies and follow-up imaging.
DBT is Improving Cancer Detection
One of the key advantages of Digital Breast Tomosynthesis (DBT) is its ability to significantly increase the detection rate of breast cancer, particularly invasive cancers, which tend to be more aggressive and require earlier intervention. Studies show that DBT can improve cancer detection rates by as much as 27% compared to traditional 2D mammography. This improvement is particularly crucial for identifying invasive cancers, which might otherwise go undetected using standard mammograms, especially in women with dense breast tissue. By providing clearer, more detailed images through its multi-angle approach, DBT enhances the ability of radiologists to catch these cancers early, when they are most treatable. Early detection is key to improving patient outcomes, as it allows for more targeted and effective treatments.
Additionally, DBT is highly effective at reducing the number of false positives, which occur when suspicious findings in traditional mammograms turn out to be benign. The precision offered by DBT significantly lowers the rate of unnecessary callbacks for further imaging or biopsies. This not only helps reduce the stress and anxiety associated with false alarms for patients but also cuts down on the financial costs linked to unnecessary follow-up procedures and tests. By minimizing false positives, DBT not only improves the overall patient experience but also contributes to cost-efficiency in breast cancer screening, benefiting both healthcare providers and patients alike.
Challenges & Adoption
Despite the clear benefits of Digital Breast Tomosynthesis (DBT), its widespread adoption has been hindered by several factors. Cost remains a significant barrier, as DBT systems are substantially more expensive than conventional mammography machines. This can limit access for smaller healthcare providers and clinics that may not have the resources to invest in the technology. In addition to the initial cost of the equipment, DBT systems require ongoing maintenance and support, further increasing operational expenses. The cost factor, combined with the need for specialised training, makes it difficult for some facilities to implement DBT, particularly in regions with limited healthcare funding.
Another concern has been the potential for increased radiation exposure compared to traditional 2D mammograms. While DBT initially raised concerns about higher radiation doses, newer systems have been able to reduce these doses to levels comparable to, or only slightly above, those of standard mammography. Additionally, modern DBT technology can now create synthesised 2D images from the 3D data, which helps minimise radiation exposure without compromising diagnostic accuracy. However, the large volume of image data generated by DBT also presents a challenge. Radiologists must undergo extensive training to interpret the complex images effectively, and healthcare facilities require advanced IT infrastructure for storage and analysis. This need for additional resources and expertise can delay widespread adoption, especially in smaller or underfunded healthcare settings.
AI Integration
The future of Digital Breast Tomosynthesis (DBT) is highly promising, with ongoing advancements designed to enhance its efficiency and accuracy. One of the most notable innovations is the creation of synthesised 2D images from the 3D data obtained during DBT. This process significantly reduces radiation exposure to patients while still maintaining the diagnostic advantages of 3D imaging. These synthesised images help eliminate the need for an additional 2D mammogram, thereby lowering the overall radiation dose without sacrificing accuracy. This makes DBT a more attractive option for both healthcare providers and patients, offering a safer yet still highly effective method for breast cancer screening
Additionally, the integration of artificial intelligence (AI) is enhancing the detection of breast cancer by assisting radiologists in analysing large volumes of data, flagging potential abnormalities, and reducing human error.
Private & NHS DBT Use
In the UK, DBT is increasingly available both privately and through the NHS, though availability can vary. Private providers like Spire Healthcare and Thames Breast Clinic offer DBT as a premium option for patients who want more detailed imaging or have dense breast tissue, which can make traditional mammograms less reliable. While the NHS offers 2D mammograms as the standard, there are efforts to expand the use of DBT across NHS facilities, especially as more studies highlight its effectiveness in early detection and reducing unnecessary callbacks.

