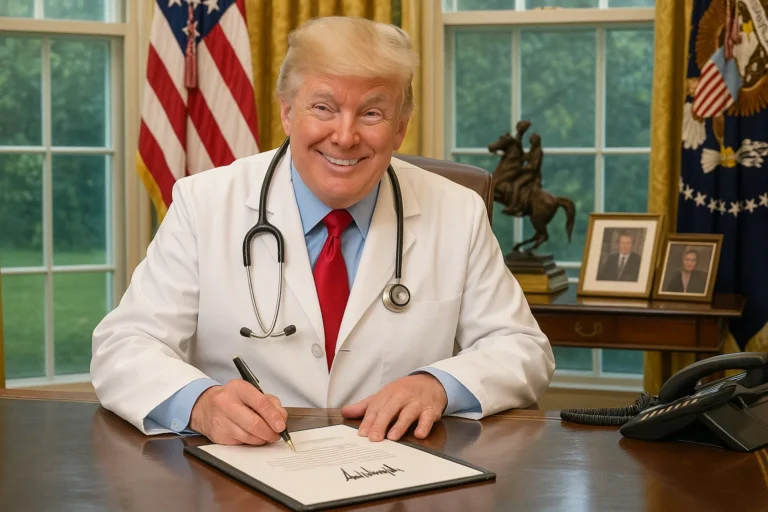
Breaking news reports have announced President Donald Trump’s signing of a sweeping executive order aimed at drastically reducing the cost of prescription medication in the United States.
The order introduces a ‘Most Favoured Nation’ pricing policy, requiring that pharmaceutical companies match the lowest prices paid for drugs in economically-advanced nations or face penalties.
Drug pricing has long been a source of public frustration, political debate, and financial hardship for many Americans.
According to the administration, the policy could reduce the cost of some high-priced drugs by as much as 90%, translating into trillions of dollars in long-term savings for consumers and public health programmes, like Medicare.
However, reports say that critics, including many in the pharmaceutical industry, warn that this strategy could disrupt drug availability, reduce incentives for innovation, and prompt legal challenges over its implementation.
The executive order comes after decades of concern over the high cost of medication in the United States. For years, Americans have paid significantly more for prescription drugs than people in other developed countries.
A 2021 RAND Corporation study found that drug prices in the U.S. were nearly 2,5 times higher than those in 32 comparable countries. This disparity has made life-saving treatments unaffordable for millions of Americans, forcing some to ration medication, skip doses, or forgo treatment altogether.
High-profile examples have only fueled public outrage. In 2015, Martin Shkreli, then-CEO of Turing Pharmaceuticals, infamously raised the price of Daraprim by more than 5 000%, from $13.50 to $750 per tablet. This is a medicine used to treat parasitic infections. The incident sparked a national debate on pharmaceutical prices.
Similarly, the cost of insulin, a drug developed nearly a century ago, has skyrocketed in recent decades. This has happened in spite of minimal changes to its formulation. Its high price has created hardships for people with diabetes who rely on it daily.
Why Are U.S. Drug Prices So High?
Several factors contribute to the persistently high cost of drugs in the United States. One of the most significant is the lack of government regulation over pricing. Unlike many other developed nations, where governments negotiate drug prices on behalf of their populations, the U.S. has traditionally allowed drugmakers to set their own prices, particularly for brand-name medications.
In addition, the American pharmaceutical market is highly fragmented, with multiple intermediaries, such as pharmacy benefit managers (PBMs), wholesalers, and insurers. These many players can result in obscured transparency and distorted pricing structures. Patents and market exclusivity further shield drugs from generic competition, allowing companies to maintain high prices even after recovering research and development costs.
Moreover, lobbying by the pharmaceutical industry has historically prevented comprehensive reforms. The industry spent over $350 million on lobbying in 2022 alone, making it the highest-spending lobbying sector in the country. As a result, efforts to allow Medicare to negotiate drug prices have repeatedly stalled in Congress.
Trump’s 2025 executive order directly challenges the pharmaceutical industry’s pricing power by tying U.S. prices to the lowest prices paid by comparable high-income countries. Dubbed the ‘Most Favoured Nation’ policy, it compels drugmakers to offer Medicare and other federal health programmes the same prices which they provide to nations like Germany, the United Kingdom, or Canada. If they fail to do so, they could face stiff penalties.
This international benchmarking model marks a significant policy departure from previous U.S. strategies, introducing a level of price negotiation the country has historically avoided. The order applies initially to a specific list of high-cost drugs administered in hospitals and clinics under Medicare Part B, but officials have indicated the policy could expand to cover retail prescription drugs under Medicare Part D in the future.
The administration estimates the change could reduce Medicare spending on select drugs by up to 90%, saving taxpayers billions of dollars annually. Patients, particularly seniors and those on fixed incomes, stand to benefit most, as out-of-pocket costs for critical medications could drop substantially.
Industry Backlash
While the executive order has been applauded by consumer advocacy groups and budget watchdogs, the pharmaceutical industry has pushed back fiercely. Drug companies argue that pegging prices to international benchmarks fails to account for the unique market dynamics of the U.S. and could hinder their ability to recoup the costs of innovation, including the lengthy and expensive process of bringing a new drug to market.
Critics also warn that the policy could lead to drug shortages or reduced access to new treatments in the U.S. if companies are unwilling to sell at the mandated prices. Some have hinted at withdrawing drugs from the Medicare market altogether, while others suggest they may raise prices abroad to offset lost revenue, potentially leading to global price inflation.
Legal challenges are also expected. Industry representatives contend that the executive order oversteps the president’s authority and violates administrative procedure laws. Lawsuits seeking to block its implementation are already being prepared, raising questions about whether the policy will survive judicial scrutiny.
The executive order was announced on May 12, 2025, and is expected to take effect in stages. The first wave of drug pricing reforms is scheduled for implementation in late 2025, with full rollout anticipated by early 2026. In the meantime, the Department of Health and Human Services (HHS) has been tasked with drafting the final rules and regulations governing enforcement.
Politically, the move bolsters President Trump’s campaign narrative, reinforcing his populist stance on issues that directly impact household budgets.
A Turning Point for U.S. Healthcare?
Whether the policy will succeed, and whether it will survive the legal and logistical hurdles ahead, remains to be seen. What is clear, however, is that the debate over drug pricing in America has reached a significant milestone.
If implemented effectively, the Most Favoured Nation policy could serve as a prototype for broader reform, potentially laying the groundwork for a more equitable and sustainable drug pricing system. It could also influence private insurers to negotiate harder and prompt manufacturers to reconsider pricing strategies across the board.
* Image generated using AI